Plantar Fasciitis (Heel Pain) Treatment
If you’re waking up with sharp heel pain or struggling with discomfort during walking, running, or standing at work, you may be dealing with plantar fasciitis. It’s one of the most common causes of heel pain—and thankfully, it responds extremely well to the right treatment plan.
At Stride Footcare in West End, Brisbane, podiatrist Cristina Smundin uses advanced assessment tools including treadmill gait analysis, BTL shockwave therapy and other modalities to diagnose the cause of your pain and guide your recovery.
This guide covers everything you need to know about plantar fasciitis, how it’s treated, and what to expect during recovery.
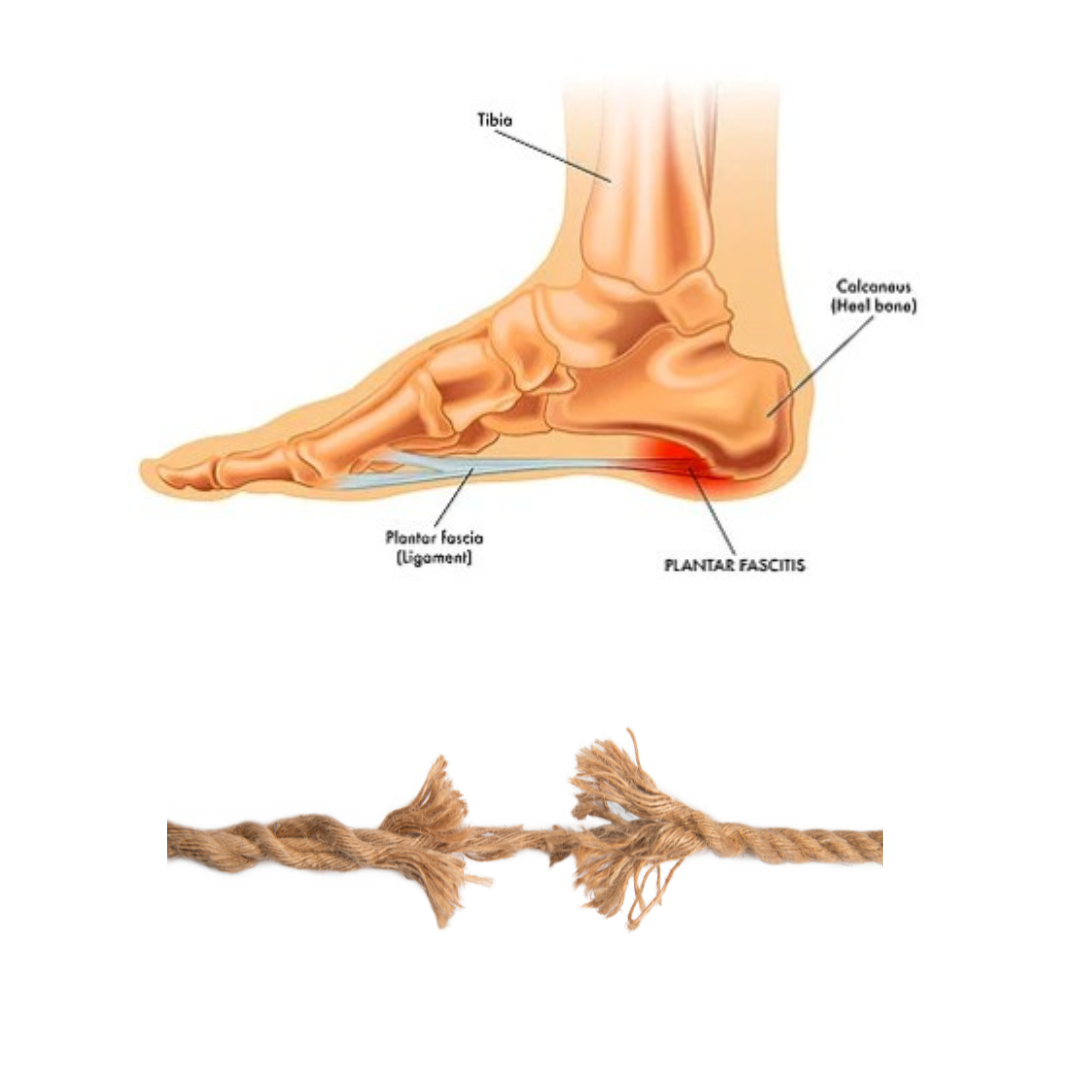
Most people think plantar fasciitis is an inflamed heel, but really it behaves more like a worn-out rope, rather than something that’s swollen and angry.
Your plantar fascia is a tough, fibrous band that’s meant to absorb load and keep your arch stable, the same way a rope supports weight.
Over time, with repeated strain, small fibres in the rope begin to fray, weaken and lose their resilience. They’re not inflamed in the classic sense. They’re simply overloaded and under-recovered.
That’s plantar fasciitis:
Not a fire that needs extinguishing, but a structure that needs time, strength and the right loading plan to repair itself.
The most common signs of plantar fasciitis include:
Sharp or stabbing pain at the bottom of the heel, especially with the first steps in the morning
Discomfort after long periods of standing or sitting
Pain that worsens with activity but eases with rest
What is Plantar Fasciitis?
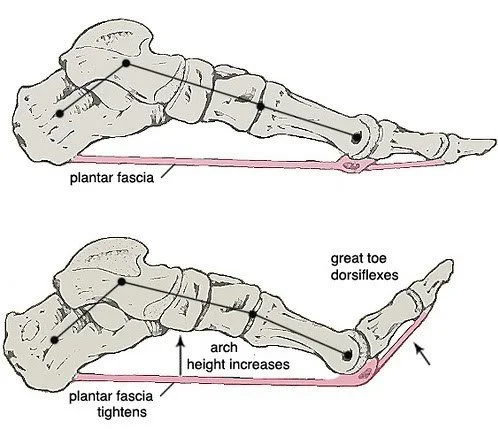
The plantar fascia:
Stabilises your arch
Acts like a shock absorber
Supports efficient walking and running
Tightens your arch (windlass mechanism) to create a stronger push-off
When overloaded, without adequate recovery and strengthening, this system becomes painful and stiff.
What the Plantar Fascia Does
Acute vs. Chronic Plantar Fasciitis
Chronic Plantar Fasciitis
Lasting >1 month
More degenerative than inflammatory
Behaves similarly to a tendinopathy
Requires progressive loading and likely shockwave therapy
Acute Plantar Fasciitis
Recent onset
More inflammatory/acute
Responds well to offloading and short-term support
Understanding the difference helps guide treatment:
Rest alone usually won’t resolve chronic cases.
Common Symptoms
Morning pain with first steps
Pain on the inside bottom of the heel
Pain after sitting or resting
Stiffness in the arch
Pain when walking barefoot
Pain increasing with walking or running
Tight calves or restricted ankle mobility
Conditions that Mimic Plantar Fasciitis
Not all heel pain is plantar fasciitis. We also check for:
Plantar fascia tear
Baxter’s nerve entrapment
Heel pad syndrome
Tarsal tunnel syndrome
Stress fractures
Bursitis
Fat pad atrophy
Achilles insertional issues
Systemic inflammatory conditions
A thorough biomechanical assessment ensures accurate diagnosis.
How We Diagnose Plantar Fasciitis
1. Consultation & Medical History
We discuss symptoms, footwear, activity load, occupation, running/training background and any previous injuries.
2. Hands-On Biomechanical Examination
Including:
Heel palpation
Fascia tension
Calf strength
Ankle range of motion
Big toe mobility
Single-leg function tests
Treadmil Gait Analysis - Walking and Running
4. Footwear Assessment
We review your current shoes to ensure they support your foot correctly.
5. Doppler Vascular Testing (If required)
Used if symptoms are atypical to rule out vascular contributors.
6. Imaging (if required)
Sometimes we refer for ultrasound, X-ray, or MRI if:
Symptoms persist
A tear is suspected
A stress fracture needs ruling out
Treatment Options for Plantar Fasciitis
We tailor treatment depending on your symptoms, lifestyle and goals.
Load Management
We adjust standing, walking and running loads to reduce irritation without completely resting (which often worsens symptoms).
Footwear Prescription
Correct footwear can immediately reduce strain on the plantar fascia.
We consider:
Heel height (pitch)
Midsole stiffness
Rocker sole (if needed)
Shock absorption/Cushioning
Appropriate sizing - Width and length
Taping
Provides short-term relief and reduces tension on the fascia.
Strengthening & Rehabilitation
A personalised program may include:
Calf raises
Plantar fascia loading
Intrinsic foot exercises
Balance and control work
Hip/glute strengthening
This is essential for long-term recovery.
Manual Therapy
May include soft tissue release, fascial work, joint mobilisation or dry needling.
Custom Foot Orthotics
Used when:
Biomechanics contribute to overload
You stand for long hours
Other treatments haven’t fully resolved symptoms
We need to put the pressure elsewhere in the foot, so the plantar fascia can heal
Your custom devices are a strong differentiator at Stride Footcare.
Shockwave Therapy (ESWT)
BTL-6000 Radial Shockwave
Shockwave therapy is one of the most effective treatments for chronic plantar fasciitis, especially when symptoms have lasted longer than 1 month.
It works by:
Increasing blood flow
Stimulating tissue healing
Reducing pain sensitivity
Promoting new collagen formation
Treatment Course
Usually 3–6 weekly sessions
Many patients notice improvement by week 2–3
Most see 50–80% improvement after 4–6 weeks
Backed by Research
Studies show shockwave therapy:
Is more effective than cortisone long-term
Significantly reduces pain in chronic cases
Works best alongside strength training
Non-invasive
We use the BTL-6000 Elite, one of the most powerful and clinically validated radial shockwave systems available.
Treatment Timeline
What to Expect over 12 weeks
Weeks 1–2
Initial assessment and outline of plan
Taping/footwear padding
Footwear review and suggestions if current footwear not appropriate
Light load program if tollerated
First 1–2 shockwave sessions
Custom Foot Orthotics if required
Weeks 3–6
Progressive strengthening
Mobility improvements
Gait and load corrections
Ongoing shockwave
50–80% improvement is typical here
Weeks 6–12
Return-to-running guidance
Building long-term capacity
If pain persists, refer to Sports Doctor or Podiatric Surgeon
Most patients are pain-free or significantly improved by this stage.
Frequently Asked Questions
Is plantar fasciitis the same as a heel spur?
No, heel spurs are caused by the plantar fascia pulling on the bone and causing an adaptation to the bone over time.
Do cortisone injections help?
They may relieve pain short-term but don’t solve the underlying problem.
Should I stretch my plantar fascia?
Over-stretching may worsen symptoms, plantar fasciitis responds well to specific exercises with increasing weight.
Do I need orthotics?
If the pain is chronic and biomechanics contribute to the cause of the pain, then custom foot orthotics are a great tool to use as part of your treatment plan.
When should I see a podiatrist?
As soon as you notice abnormal heel pain